
South Australian Medical Heritage Society Inc
Website for the Virtual Museum
Home
Coming meetings
Past meetings
About the Society
Main Galleries
Medicine
Surgery
Anaesthesia
X-rays
Hospitals,other organisations
Individuals of note
Small Galleries
Ethnic medicine
- Aboriginal
- Chinese
- Mediterran
The History of Peptic Ulceration
ACKNOWLEDGEMENTS
We are most grateful to Prof Ian Roberts-Thomson for this article, which is based on his presentation on “The History of Peptic Ulceration” given to the Society in February, 2017.
THE HISTORY OF PEPTIC ULCERATION
Surprisingly, gastric and duodenal ulcers (peptic ulcers} appeared to be rare before the 19th century. This conclusion was largely based on a very low frequency of perforated ulcers which were a recognized cause of severe abdominal pain followed by death after 1 or 2 days. However, by the end of the 19th century, perforated duodenal ulcers were increasingly recognized, particularly in men. In the first half of the 20th century, ulcers were estimated to affect up to 10% of the adult population with significant morbidity and mortality from complications such as gastrointestinal bleeding and perforation. However, the second half of the 20th century has seen a progressive fall in the incidence of ulcers, particularly duodenal ulcers, in both developed and developing countries.
Although several authors contributed to an understanding of the composition of gastric juice, none was more important than the observations of William Beaumont (1785-1853) on the gastric secretions of his patient with a gastric fistula. Beaumont confirmed the presence of muriatic (hydrochloric) acid and documented several other functions of the stomach including motility, digestion and responses to meals and common drinks.
The period 1850-1900 was dominated by surgeons. Chloroform and ether anesthetics were available and upper gastrointestinal surgery was developed to treat pyloric obstruction and perforated ulcers. The most prominent surgeon in Europe was Theodore Billroth (1829-1894) who developed operative procedures for removal of the lower stomach that still retain his name. Some surgeons felt that the beneficial effects of surgery were related to a reduction in gastric acid and a German surgeon, Karl Schwarz, coined the term “no acid, no ulcer” in 1910.

1829 - 1894
The first half of the 20th century was dominated by the study of gastric acid secretion. Following passage of a nasogastric tube, acid was measured in the basal state (usually for 1 hour) and after stimulation with a derivative of histamine called Histalog (again for 1 hour). Although there was overlap between duodenal ulcer patients and controls, most studies showed that ulcer patients had higher mean acid outputs, both in the basal state and after stimulation with Histalog. Other studies attributed this to increased numbers of acid-producing cells (parietal cells) in the upper stomach. Men also tended to produce more acid than women and smoking (largely men) was established as a risk factor for ulcers. Another surgeon, Lester Dragstedt (1893-1975), confirmed the role of the vagus nerve in gastric acid secretion in dogs and subsequently pioneered the use of truncal vagotomy for the surgical treatment of duodenal ulcers. As truncal vagotomy impaired gastric emptying, the surgery was modified to widen the aperture of the pylorus (pyloroplasty). Later operations called selective vagotomies divided only those branches of the vagus nerve that supplied the acid-producing part of the stomach. Most of these operations avoided the need for pyloroplasty.

1893 - 1975
Another aspect of gastric acid secretion was highlighted by US surgeons, Robert Zollinger and Edwin Ellison, in 1955. They described nine patients with recurrent ulcers despite surgery who had islet cell tumors of the pancreas. They postulated that the tumors were producing a hormone that stimulated gastric acid secretion; a hormone that was identified as gastrin in 1968. Serum levels of gastrin were extremely high in the Zollinger-Ellison syndrome but were also somewhat elevated in patients with ordinary duodenal ulcers.
Along with the era of gastric acid was the development of methods for the diagnosis of peptic ulcers. Although rigid tubes with light sources have been passed into the stomach since at least 1868, technical issues would have prevented the diagnosis of ulcers in the majority of patients. A more reliable method was the introduction of the barium meal radiograph in 1910. The test utilized the high density of barium sulphate that impeded the passage of X-rays creating a white appearance in the lumen of the gastrointestinal tract against a largely black background. At least one difficulty was differentiating active ulceration from previous ulceration with scarring, particularly in the duodenal cap. This was largely overcome by the introduction of flexible endoscopy in the late 1960's and early 1970's; equipment that provided a clear view of almost all the upper gastrointestinal tract. Initially, these flexible endoscopes were based on fiber-optic technology but, in the 1980's, these were replaced by video endoscopes producing images on a television screen.
The 1970's and 1980's were important for the development of new drugs. The first group were the histamine (H2) receptor antagonists, first developed by James Black (1924-2010) for the pharmaceutical company Smith, Kline and French. Cimetidine was launched in the mid-1970's and, for a time, became the largest-selling prescription drug in the world. Other H2 receptor antagonists, including ranitidine, were developed by different companies and were also highly successful products. Overall, H2 receptor antagonist drugs reduced gastric acid secretion by approximately 60% and healed almost all peptic ulcers. The second group of drugs targeted the acid-secreting pump at the apex of the parietal cell and were commonly known as proton-pump inhibitors. The first of these drugs, omeprazole, was developed by Astra Pharmaceuticals and decreased acid production by at least 80%. Again, this was associated with accelerated ulcer healing as well as effective control of reflux oesophagitis.
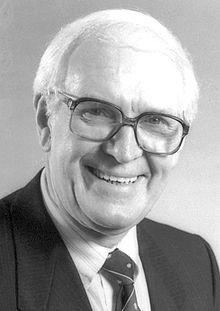
1924 - 2010
The potential role of bacteria in peptic ulceration was reawakened by Robin Warren, a pathologist in Perth. He noted that curved bacteria were often present in resected gastric specimens from patients who had operations for peptic ulceration. In 1981, he persuaded a medical registrar, Barry Marshall, to assist with the collection of clinical data. Together, they established the relationship between Campylobacter pylori (later called Helicobacter pylori) and peptic ulceration, cultured the bacteria on special media and showed that infection with H. pylori could cause gastritis. Subsequently, they developed drug regimens for the treatment of H. pylori and developed tests for the diagnosis of infection based on the ability of the organism to produce a particular enzyme called urease. They received the Nobel Prize for Medicine in 2005.
The current treatment for peptic ulceration now includes eradication of H. pylori. If this is successful, the risk of recurrent ulceration is low. Eradication of H. pylori also results in a reduction in gastric acid secretion and normalization of serum gastrin levels. The relationship between H. pylori and gastric acid secretion is still debated but one possibility is that infection in the lower stomach decreases levels of a hormone called somatostatin that normally impairs the release of gastrin. Another issue is an explanation for the emergence of peptic ulceration late in the 19th century. This may involve a change in the age of exposure to H. pylori. For example, prior to the 19th century, exposure to H. pylori may well have occurred early in life when immune responses were under-developed. This may have favored a more diffuse infection with involvement of the upper stomach (with impaired acid secretion) as well as involvement of the lower stomach. With advances in hygiene and water safety, exposure to H. pylori may have been delayed for some years. This would favor a more effective immune response that might restrict infection to the lower stomach with minimal damage to the upper stomach and enhanced gastric acid secretion in response to higher levels of gastrin. If this is the case, peptic ulceration could be categorized as another disease of civilization, albeit one that will largely disappear with decreasing exposure to H. pylori as well as the greater use of effective therapy.
Ian Roberts-Thomson
Emeritus Professor, University of Adelaide.
March, 2017